Introduction
- Overview of Microneedling
- Historical Background
- Scope of the Manual
Chapter 1: Scientific Principles and Mechanism of Action
- The Skin’s Anatomy and Physiology
- Mechanism of Microneedling
- Collagen Induction Therapy
- Effects on Skin Rejuvenation and Scar Treatment
Chapter 2: Indications and Contraindications
- Indications for Microneedling
- Contraindications and Precautions
- Patient Selection Criteria
Chapter 3: Pre-procedure Evaluation and Preparation
- Patient Consultation and Informed Consent
- Skin Assessment
- Pre-treatment Guidelines
- Required Equipment and Materials
Chapter 4: Microneedling Techniques
- Types of Microneedling Devices
- Manual Devices
- Automated Pen Devices
- Depth of Penetration and Treatment Parameters
- Technique Variations for Specific Conditions
- Acne Scars
- Hyperpigmentation
- Anti-Aging: Wrinkles and Fine Lines
- Stretch Marks
- Alopecia
Chapter 5: Procedure Protocols
- Sterilization and Safety Standards
- Step-by-Step Procedure Guide
- Pain Management Strategies
- Handling Sensitive Skin Areas
Chapter 6: Post-procedure Care and Patient Instructions
- Immediate Post-procedure Care
- Homecare Instructions for Patients
- Managing Side Effects and Complications
- Follow-up Schedule
Chapter 7: Combination Therapies and Advanced Techniques
- Combining Microneedling with Topical Treatments
- Integration with Other Aesthetic Procedures (e.g., PRP, Lasers)
- Recent Advances and Research Insights
Chapter 8: Practice Management and Ethical Considerations
- Incorporating Microneedling Services into Practice
- Expert Commentary and Best Practices
- Setting Patient Expectations
- Legal and Ethical Issues in Cosmetic Dermatology
References
Introduction
Microneedling, also known as collagen induction therapy, is a minimally invasive dermatological procedure that has gained mainstream acceptance in the field of aesthetic medicine for its effectiveness in skin rejuvenation, scar treatment, and various other skin conditions. This manual provides medical professionals with a comprehensive guide to the principles, practices, and patient care involved in microneedling, based upon the latest research and clinical evidence.
Overview of Microneedling
Microneedling involves the use of fine, short, sterile needles to create micro-injuries on the skin surface. These micro-injuries initiate a natural wound healing process that enhances collagen and elastin production, leading to improved skin texture, firmness, and hydration. Over the past decade, microneedling has evolved into a versatile treatment modality for addressing a wide range of skin concerns, such as acne scars, wrinkles, fine lines, stretch marks, and alopecia.
Historical Background
Using needles to rejuvenate the skin dates before the 1990s, but it wasn’t until the early 2000s that microneedling devices became commercially available and widely adopted by aesthetic practitioners. Microneedling techniques have been supported by a growing body of clinical research that demonstrates its safety and efficacy compared to more invasive cosmetic procedures.
Scope of the Manual
This manual is designed to serve as an essential resource for medical practitioners, providing in-depth knowledge on the scientific basis of microneedling, practical guidelines for its application, and insights into patient management. By integrating findings from pivotal studies and expert recommendations, the manual addresses key aspects of microneedling practice enabling practitioners to deliver optimal results while ensuring patient safety and satisfaction.
Chapter 1: Scientific Principles and Mechanism of Action
The Skin’s Anatomy and Physiology
The skin, the largest organ of the human body, serves as a protective barrier against mechanical, thermal, and physical injury and hazardous substances. It also regulates temperature, controls evaporation, and plays a vital role in sensory perception. Structurally, the skin is divided into three primary layers: the epidermis, dermis, and hypodermis (subcutaneous tissue).
- Epidermis: The outermost layer, responsible for the barrier function and skin tone.
- Dermis: The middle layer, containing dense, irregular connective tissue that houses collagen and elastin fibers, providing strength, flexibility, and elasticity to the skin.
- Hypodermis: The deeper subcutaneous tissue, primarily involved in fat storage and providing insulation and cushioning for the skin.
These layers contributes to the skin’s overall health, appearance, and its ability to repair and regenerate.
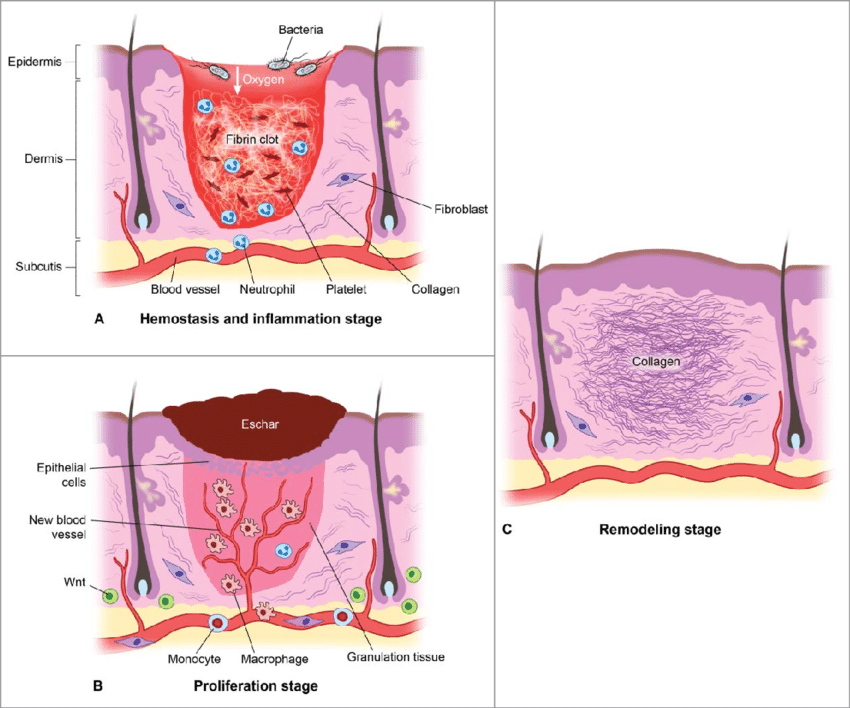
Mechanism of Microneedling
Microneedling works by creating controlled micro-injuries to the skin, which trigger the body’s wound healing processes. This procedure is performed using a device equipped with fine needles that puncture the skin to various depths ranging from 0.5mm to 2.5mm. These micro-injuries stimulate the release of growth factors and induce collagen and elastin production without causing significant damage to the epidermis.
Collagen Induction Therapy
The primary mechanism through which microneedling exerts its effects is known as Collagen Induction Therapy (CIT). CIT promotes the remodeling of existing collagen and increases the formation of new collagen and elastin fibers. The process begins with the inflammation phase, where platelets release growth factors that lead to the formation of new fibroblasts. The proliferation phase follows, where fibroblasts are transformed into collagen. Finally, the remodeling phase sees the maturation of collagen, which tightens the skin and improves its texture and appearance.
Effects on Skin Rejuvenation and Scar Treatment
- Skin Rejuvenation: Microneedling is effective in improving skin texture, reducing fine lines and wrinkles, and increasing skin elasticity. By promoting the production of collagen and elastin, microneedling can enhance the skin’s appearance, making it look firmer, smoother, and more youthful.
- Scar Treatment: Microneedling is particularly beneficial for the treatment of acne scars, surgical scars, and stretch marks. It works by breaking down old scar tissue and stimulating the synthesis of new collagen fibers, aligned more regularly compared to the disorganized collagen in scar tissue. This process not only reduces the appearance of scars but also helps in normalizing the skin’s texture and color.
Multiple studies have demonstrated the efficacy of microneedling in both skin rejuvenation and scar treatment. It has been shown to improve skin texture, reduce the severity of scars, and enhance the overall appearance of the skin with minimal downtime and side effects.
Chapter 2: Indications and Contraindications
Indications for Microneedling
Microneedling has been studied extensively and proven effective for various dermatological conditions, offering benefits across a wide spectrum of skin concerns:
- Acne Scars: Reduces the appearance of atrophic acne scars.
- Skin Rejuvenation: Improves skin texture and a reduction in fine lines and wrinkles.
- Melasma: Improves Melasma Area and Severity Index (MASI) scores and reduces melasma (NOTE: While microneedling has shown promise in treating melasma, its efficacy is still under debate. Some studies have reported improvements in MASI scores, but others have not. More research is needed to definitively confirm its effectiveness for melasma).
- Stretch Marks (Striae): Remodels scar tissue and enhanced the color and texture of stretch marks.
- Alopecia: Enhances the penetration of topical treatments and stimulates hair follicle growth (NOTE: Microneedling has been investigated as a potential treatment for alopecia, but its effectiveness is not yet fully established. Some studies have reported positive results, but more research is needed to confirm its efficacy and determine the optimal treatment parameters).
- Skin Tightening: Enhances skin elasticity and firmness.
- Scar Reduction: Promotes the remodeling of scar tissue and improving cosmetic appearance.
Contraindications
- Keloid Scars: History of or tendency to form keloid scars is a contraindication due to the risk of exacerbating scar formation.
- Active Eczema: Including other active dermatitis forms, as microneedling may worsen the condition.
- Psoriasis and Chronic Skin Diseases: Moderate to severe chronic skin diseases such as psoriasis, which may be aggravated by microneedling.
- History of Specific Skin Conditions: Such as actinic or solar keratosis and herpes simplex infections, which pose a risk of flare-ups and complications.
- Raised Moles: Presence of raised moles in the treatment area, which should be avoided to prevent irritation or transformation. Caution should be exercised, and it’s best to consult with a dermatologist beforehand.
- Blood Disorders: Including blood dyscrasias and patients on anticoagulant therapy, due to the increased risk of bleeding and bruising.
- Ongoing Cancer Treatments: Patients currently undergoing chemotherapy or radiotherapy, as their immune response and healing capacity may be compromised.
- Immunosuppression: Including conditions such as scleroderma, collagen or vascular diseases, cardiac abnormalities, and those on immunosuppressive therapy, which increase the risk of adverse reactions.
- Active Infections: Bacterial, viral, or fungal infections in the treatment area increase the risk of spreading the infection and delaying healing.
- Blood Clotting Disorders: Including hemophilia, due to the increased risk of prolonged bleeding.
- Active Acne and Infections: Especially inflammatory lesions and localized infections such as warts and herpes labialis, which could be exacerbated by the procedure.
- Pregnancy and Nursing: Microneedling is not recommended for pregnant or nursing women due to a lack of safety data and potential risks to the fetus or infant.
Precautions
- Comprehensive Health Disclosure: Patients must disclose all health conditions, medications, supplements, and lifestyle factors that could impact the microneedling procedure.
- Prophylactic Antiviral Therapy: For patients prone to herpes simplex, prophylactic antiviral therapy is recommended to prevent outbreaks.
- Diabetes Management: Patients with diabetes should be informed of potential delayed wound healing and monitored accordingly.
- Skin Pigmentation Management: Patients with darker skin tones or those prone to PIH should pre-treat with a melanin-inhibiting regimen for at least 2 weeks prior to treatment.
- Assessment of Suspicious Lesions: Any suspicious lesions must be evaluated and diagnosed by a dermatologist prior to treatment to rule out malignancies.
- Discontinuation of Certain Therapies: Autoimmune therapies and retinoid products should be discontinued 24 hours before the procedure to reduce the risk of adverse reactions.
- Avoidance of Active Inflammatory Conditions: Do not perform microneedling over active acne, rosacea, or other inflammatory skin conditions to prevent exacerbation.
- Avoidance of Open Wounds: Microneedling should not be performed over open wounds or sores to prevent infection and further damage.
- Sensitive Area Restrictions: The device should not be used inside the orbital rim or within the vermillion border of the lips due to the delicate nature of these areas.
- Viral Outbreak Prophylaxis: Consider antiviral prophylaxis for patients with a history of frequent viral infections.
- Post-Accutane Treatment: Microneedling should not be administered for at least 6 months following the use of isotretinoin (Accutane) due to the increased risk of scarring and delayed wound healing.
- Medical History Review: Patients must complete a comprehensive Medical History Form prior to treatment to assess suitability and minimize risks.
Patient Selection Criteria
Selecting the right candidates for microneedling involves assessing the patient’s skin condition, medical history, and treatment goals.
Risks
Every medical procedure involves inherent risks and potential complications. It is crucial to understand these risks and weigh them against the potential benefits of microneedling. Although most patients experience minimal adverse effects, it is important to discuss these risks with your provider to ensure informed consent.
- Skin Irritation and Erythema: Common immediately post-treatment, presenting as erythema resembling a mild sunburn, which typically resolves within a few days due to the inflammatory response induced by microneedling.
- Edema: Mild to moderate localized swelling can occur, particularly in sensitive areas, and usually subsides within a few days as part of the body’s healing process.
- Ecchymosis: Bruising may occur depending on the patient’s skin sensitivity and the intensity of the treatment, resulting from minor vascular trauma.
- Dry Skin and Desquamation: The skin may become dry and undergo desquamation as it heals, a normal part of the regenerative process facilitated by microneedling.
- Infection: Although rare, there is a risk of bacterial, viral, or fungal infection if post-treatment care instructions are not strictly followed, due to the creation of micro-channels in the skin.
- Hemorrhage: Minor bleeding during the procedure is possible, especially with deeper needle penetration, which can be managed with appropriate pressure and hemostatic measures. Hemorrhage is a rare complication of microneedling, and significant bleeding is uncommon.
- Pain: Patients may experience discomfort during and immediately after the procedure; severe pain is uncommon and should be promptly reported.
- Post-inflammatory Hyperpigmentation (PIH): There is a risk of PIH, particularly in individuals with darker skin tones or those exposed to sunlight without adequate protection, due to melanocyte activation.
- Hypopigmentation: Less common than hyperpigmentation, but there is a risk of depigmented patches forming post-treatment as a result of melanocyte disruption.
- Scarring: Rare, but possible, especially in individuals with a history of keloids or hypertrophic scarring, due to abnormal wound healing responses.
- Allergic Reactions: Possible reactions to topical anesthetics, serums, or other products applied during or after the procedure.
- Herpes Simplex Virus Reactivation: Patients with a history of herpes simplex may experience reactivation and outbreaks following the treatment due to the trauma-induced stress response.
- Acneiform Eruptions: Post-treatment acneiform eruptions can occur, likely due to follicular occlusion and the skin’s inflammatory response.
- Unsatisfactory Aesthetic Results: There is a risk that the cosmetic outcomes may not meet patient expectations, highlighting the importance of setting realistic goals.
- Textural Changes: Some patients may observe changes in skin texture, including areas of roughness or unevenness, during the healing process.
- Increased Sensitivity to Topicals: Post-procedure, the skin may exhibit heightened sensitivity to skincare products, necessitating adjustments in the patient’s regimen.
- Photosensitivity: Enhanced sensitivity to UV radiation post-treatment necessitates the use of broad-spectrum sunscreens and avoidance of direct sunlight to prevent adverse effects.n
Patients should be thoroughly evaluated to identify any contraindications and to discuss potential risks and benefits. A detailed medical history, including medication use, history of skin diseases, and previous cosmetic procedures, should be obtained to ensure patient safety and optimize treatment outcomes.
Chapter 3: Pre-procedure Evaluation and Preparation
Patient Consultation and Informed Consent
Before proceeding with microneedling, a detailed patient consultation is essential to establish treatment goals, discuss expectations, and review the patient’s medical history. This consultation should cover the procedure’s benefits, potential risks, and side effects. Informed consent is a critical component, ensuring that the patient understands the procedure, possible outcomes, and any associated risks.
Skin Assessment
A thorough skin assessment should be conducted to evaluate the patient’s skin type, identify target areas for treatment, and detect any contraindications, such as active infections or inflammatory conditions. This assessment guides the selection of appropriate microneedling depth and technique, tailored to the patient’s specific skin concerns and objectives.
Pre-treatment Guidelines
Pre-treatment preparation is crucial for optimizing outcomes and minimizing complications. Recommendations typically include:
- Medical History:
- Complete and submit a detailed medical history form.
- Disclose all medications, supplements, and health conditions.
- Medications and Topicals:
- Discontinue use of retinoids, Retin-A, and exfoliating agents (AHAs, BHAs) at least 48 hours before treatment.
- Stop use of Accutane (isotretinoin) for at least 6 months before treatment (NOTE: While it is generally recommended to wait a period of time after stopping isotretinoin before undergoing microneedling, the exact duration can vary depending on individual factors and the specific type of microneedling being performed. Some studies suggest that a shorter interval may be acceptable in certain cases, but it’s crucial to consult with a dermatologist to assess the individual’s skin condition and determine the appropriate waiting period).
- Avoid blood-thinning medications (e.g., aspirin, ibuprofen) and supplements (e.g., fish oil, vitamin E) 5-7 days before treatment.
- Sun Exposure:
- Avoid direct sun exposure, tanning beds, and self-tanning products for at least 2 weeks before treatment.
- Use a broad-spectrum SPF 30 or higher sunscreen daily.
- Skin Care:
- Cleanse the treatment area thoroughly on the day of the procedure.
- Do not use any harsh skin care products or undergo other skin treatments (e.g., chemical peels, laser treatments) for at least 1 week before microneedling.
- Health and Wellness:
- Stay hydrated by drinking plenty of water.
- Avoid alcohol consumption for at least 24 hours before treatment.
- Do not shave the treatment area on the day of the procedure to avoid skin irritation.
- Prophylactic Treatments:
- Consider taking antiviral medication if you have a history of herpes simplex to prevent an outbreak.
- Patients with a history of keloids or abnormal wound healing should discuss this with their practitioner.
- Other Considerations:
- Arrange for transportation if you are prone to anxiety or discomfort and plan to take a sedative.
- Wear comfortable clothing that allows easy access to the treatment area.
Required Equipment and Materials
The equipment and materials needed for a microneedling session include:
- Microneedling Device: A sterile, FDA-approved microneedling device, such as a dermaroller or a motorized pen, chosen based on the treatment area and specific skin concerns.
- Topical Anesthesia: A topical anesthetic cream, typically lidocaine, applied to the treatment area 30-60 minutes before the procedure to minimize discomfort.
- Antiseptic Solution: To cleanse the skin before the procedure and reduce the risk of infection.
- Sterile Saline Solution: For cleaning the skin during the procedure.
- Hydrating and Healing Topicals: Application of hyaluronic acid, growth factors, or peptide solutions post-procedure to enhance healing and moisturize the skin.
- Protective Equipment: Including gloves, masks, and sometimes goggles for the practitioner to ensure a sterile environment and prevent any contamination.
Chapter 4: Microneedling Techniques
Types of Microneedling Devices
Microneedling devices are designed to puncture the skin to create controlled micro-injuries, stimulating the body’s natural wound healing process. There are primarily two types of microneedling devices: manual and automated pen devices.
- Manual Devices: Manual devices, such as dermarollers, consist of a rolling drum lined with microneedles. These devices are rolled over the skin to create micro-injuries. The depth of needle penetration is fixed and depends on the needle length of the device. Dermarollers are simple to use and cost-effective, making them a popular choice for home use.
- Automated Pen Devices: Automated pen devices use electric or battery power to rapidly puncture the skin with microneedles. The depth of penetration can be adjusted, allowing for more precise control over the treatment. These devices are considered more efficient and can reduce treatment time, especially for large or contoured areas of the skin making it ideal for use in the clinic.
Depth of Penetration and Treatment Parameters
The depth of needle penetration during microneedling is a critical factor that influences the treatment’s efficacy. It varies based on the target condition, skin type, and area being treated. As a general guideline:
- Superficial treatments (e.g., for fine lines, mild hyperpigmentation) may use needle lengths of 0.5mm to 1.0mm.
- Moderate treatments (e.g., for deeper wrinkles, moderate acne scars) often require needle lengths of 1.0mm to 1.5mm.
- Deep treatments (e.g., for severe acne scars, deep wrinkles, stretch marks) may use needle lengths of 1.5mm to 2.5mm.
Treatment parameters, including the speed of the device (for automated pens), number of passes over the treatment area, and frequency of treatment sessions, are also tailored to individual patient needs and response to treatment.
Technique Variations for Specific Conditions
Different skin conditions benefit from tailored microneedling techniques, including variations in needle depth and treatment protocols.
- Acne Scars
- Hyperpigmentation
- Anti-Aging/ Wrinkles and Fine Lines
- Stretch Marks
- Alopecia
Acne Scar Treatment Procedure Guide
| Region | Dermal (Pinpoint Blood/Proliferative Response) Average Depth Guide* |
| Forehead | 1.0 mm – 1.5 mm |
| Chin & Jawline | 1.5 mm – 2.0 mm |
| Cheeks | 1.5 mm – 2.0 mm |
| Peri-orbital | 0.25 mm – 0.5 mm |
| Nose | 1.0 mm – 1.5 mm |
| Peri-oral | 1.0 mm – 1.5 mm |
*These guides are suggestions based on the average skin response of typical patients. Adjust the needle depth as necessary to achieve the required visual endpoint.
Treatment Protocol Overview
Treatment Endpoint
- Pinpoint bleeding (papillary/reticular dermis).
Treatment Intervals
- Every 4-6 weeks
Treatment Course
- 4-6 treatments or until desired results are achieved. Maintenance treatments may be performed as necessary.
Other Considerations
- Collagen Induction:
- Microneedling stimulates fibroblast activity, promoting collagen production, which helps to fill in and smooth out atrophic scars over time.
- Skin Remodeling:
- The micro-injuries caused by microneedling initiate the skin’s natural healing process, leading to skin remodeling and scar improvement.
- Depth of Penetration:
- Deeper needle penetration is often necessary for treating acne scars, particularly ice pick and boxcar scars, to reach the deeper layers of the dermis where collagen remodeling is needed.
- Patient Variability:
- Individual responses to microneedling can vary. It’s important to monitor the patient’s progress and adjust the treatment plan as needed.
Hyperpigmentation Treatment Procedure Guide
| Region | Superficial Epidermal (No Blood/Inflammatory Response) Average Depth Guide* | Epidermal Junction/Superficial Dermal (Occasional Pinpoint Blood/Proliferative Response) Average Depth Guide* |
| Forehead | 0.3 mm | 0.4 mm |
| Chin & Jawline | 0.5 mm | 0.7-0.8 mm |
| Cheeks | 0.7 mm | 1.0 mm |
| Peri-orbital | 0.2 mm | 0.3 mm |
| Nose | 0.4 mm | 0.5 mm |
| Peri-oral | 0.4 mm | 0.5 mm |
| Body | 0.5 mm | 0.7 – 1.0 mm |
*These guides are suggestions based on the average skin response of typical patients. Adjust the needle depth as necessary to achieve the required visual endpoint.
Treatment Protocol Overview
Treatment Endpoint
- Epidermal Pigmentation: No blood, red skin (stratum spinosum/basal layer).
- Mixed and Dermal Melasma: Occasional pinpoint blood (epidermal junction/superficial papillary dermis). Reduce needle depth if consistent pinpoint blood is observed.
Treatment Intervals
- Every 2-4 weeks
Treatment Course
- 4-6 treatments or until desired results are achieved. Maintenance treatments may be performed as necessary.
Other Considerations
- Persistent and Recurring Conditions:
- Conditions like melasma are persistent and may recur. A maintenance program is necessary.
- Melanocyte Location:
- Melanocytes are located in the basal layer of the epidermis. Melanosome transfer to keratinocytes occurs in the stratum spinosum layer. Treatments should induce a superficial inflammatory response to achieve regulation and correction.
- Depth for Melasma:
- For dermal and mixed melasma, slightly deeper needle penetration is required to target affected melanophages.
Anti-Ageing Treatment Procedure Guide
| Region | Dermal (Pinpoint Blood/Proliferative Response) Average Depth Guide* |
| Forehead | 0.5 mm – 0.6 mm |
| Chin & Jawline | 1.0 mm – 1.25 mm |
| Cheeks | 1.25 mm – 1.5 mm |
| Peri-orbital | 0.3 mm – 0.4 mm |
| Nose | 0.7 mm |
| Peri-oral | 0.7 mm |
*These guides are suggestions based on the average skin response of typical patients. Adjust the needle depth as necessary to achieve the required visual endpoint.
Treatment Protocol Overview
Treatment Endpoint
- Pinpoint bleeding (papillary/reticular dermis).
Treatment Intervals
- Every 6-8 weeks
Treatment Course
- 4-6 treatments or until desired results are achieved. Maintenance treatments may be performed as necessary.
Other Considerations
- UV Exposure and Glycation:
- Ultra violet exposure is a major cause of extrinsic aging. Glycation is another major cause of intrinsic collagen degradation. Both triggers may be successfully managed via daily application and reapplication of broad-spectrum sunscreen and consuming foods with a low glycemic index.
- Collagen and Melanogenesis:
- Microneedling procedures stimulate fibroblast activity, resulting in increased collagen production, while melanogenesis becomes rebalanced. This results in visibly plumper and more even-toned skin.
Stretch Mark Treatment Procedure Guide
| Region | Dermal (Pinpoint Blood/Proliferative Response) Average Depth Guide* |
| Abdomen | 1.5 mm – 2.0 mm |
| Thighs | 1.5 mm – 2.0 mm |
| Buttocks | 1.5 mm – 2.0 mm |
| Breasts | 1.0 mm – 1.5 mm |
*These guides are suggestions based on the average skin response of typical patients. Adjust the needle depth as necessary to achieve the required visual endpoint.
Treatment Protocol Overview
Treatment Endpoint
- Pinpoint bleeding (papillary/reticular dermis).
Treatment Intervals
- Every 4-6 weeks
Treatment Course
- 4-6 treatments or until desired results are achieved. Maintenance treatments may be performed as necessary.
Other Considerations
- Collagen Induction:
- Microneedling stimulates fibroblast activity, promoting collagen production, which helps to reduce the appearance of stretch marks over time.
- Skin Remodeling:
- The micro-injuries caused by microneedling initiate the skin’s natural healing process, leading to skin remodeling and improved texture.
- Depth of Penetration:
- Deeper needle penetration is often necessary for treating stretch marks to reach the deeper layers of the dermis where collagen remodeling is needed.
- Patient Variability:
- Individual responses to microneedling can vary. It’s important to monitor the patient’s progress and adjust the treatment plan as needed.
- Maintenance:
- Stretch marks can be persistent and may require ongoing maintenance treatments to sustain the results.
Alopecia Treatment Procedure Guide
| Region | Dermal (Pinpoint Blood/Proliferative Response) Average Depth Guide* |
| Frontal | 0.5 mm – 1.0 mm |
| Vertex | 1.0 mm – 1.5 mm |
| Occipital | 1.0 mm – 1.5 mm |
| Temporal | 0.5 mm – 1.0 mm |
*These guides are suggestions based on the average skin response of typical patients. Adjust the needle depth as necessary to achieve the required visual endpoint.
Alopecia Treatment Protocol Overview
Treatment Endpoint
- Pinpoint bleeding (papillary/reticular dermis).
Treatment Intervals
- Every 4-6 weeks
Treatment Course
- 6-8 treatments or until desired results are achieved. Maintenance treatments may be performed as necessary.
Other Considerations
- Hair Follicle Stimulation:
- Microneedling stimulates dermal papillae and promotes the proliferation of hair follicle cells, aiding in the regrowth of hair.
- Topical Application:
- The microchannels created by microneedling enhance the absorption of topical treatments such as minoxidil and growth factor serums, increasing their efficacy.
- Patient Variability:
- Individual responses to microneedling can vary. It’s important to monitor the patient’s progress and adjust the treatment plan as needed.
- Maintenance:
- Alopecia can be a chronic condition, and ongoing maintenance treatments may be required to sustain hair regrowth.
Chapter 5: Procedure Protocols
Sterilization and Safety Standards
Ensuring the highest standards of sterilization and safety is essential in microneedling procedures to prevent infection and cross-contamination. All microneedling devices, whether manual or automated, must be sterilized according to manufacturer instructions. Single-use, disposable needle cartridges are recommended for automated devices to ensure safety. The work area and the practitioner’s hands must be sanitized thoroughly, and gloves should be worn throughout the procedure.
Step-by-Step Procedure Guide
Preparation and Setup
- Suitability Assessment:
- Confirm patient suitability for treatment based on medical history and skin assessment.
- Discuss any potential risks, complications, and expected outcomes with the patient.
- Organize Supplies:
- Prepare all necessary supplies on a sterile trolley: microneedling pen, disposable needle cartridges, sterile gloves, cleansing solutions, anesthetic cream, serums, gauze, calming mask, repair cream, and sunblock.
- Hand Hygiene:
- Wash hands thoroughly with soap and water before beginning the procedure.
- Patient Positioning:
- Position the patient in a semi-reclining position for optimal access to the treatment area.
Cleansing and Anesthetic Application
- Cleanse Treatment Area:
- Cleanse the treatment area with a gentle, non-alcoholic cleanser to remove makeup, oil, and debris.
- Apply Anesthetic Cream:
- Apply a thin layer of anesthetic cream to the treatment area. Follow the manufacturer’s instructions for contact time on the skin.
- Cover the area with plastic wrap to enhance absorption if recommended.
- Remove Anesthetic Cream:
- After the appropriate time, remove the anesthetic cream using sterile gauze and isopropyl alcohol. (NOTE: While isopropyl alcohol is commonly used as an antiseptic, it can be drying and irritating to the skin, especially before a microneedling procedure. Some authors recommend a gentle cleanser or sterile saline solution to remove the anesthetic cream.)
- Allow the area to dry completely.
Treatment Protocol
- Photographic Documentation:
- Take pre-treatment photographs of the treatment area for documentation and comparison.
- Serum Application:
- Apply a chosen serum (e.g., hyaluronic acid) to the treatment area to aid the glide of the microneedling pen and enhance treatment efficacy.
- Prepare Microneedling Device:
- Use a new, disposable needle cartridge. Check the expiry date on the sealed pouch.
- Insert the needle cartridge into the pen and ensure the handpiece is protected with a disposable sleeve or film.
- Treatment Technique:
- Starting Point: Begin on the cheeks to allow the patient to acclimate to the sensation.
- Needle Depth Adjustment: Adjust the needle depth for different areas (e.g., bony areas require shallower depths).
- Methods: Employ stroking, circular, and stamping techniques based on the treatment area. Ensure the pen is perpendicular to the skin.
- Movement: Hold the pen like a pencil and move it in a light, even rhythm. Use horizontal, vertical, and oblique passes, repeating each pass 3-6 times or until fine pinpoint bleeding is observed. The number of passes and the observation of pinpoint bleeding can vary depending on the individual’s skin, the treatment area, and the specific goals of the procedure. While pinpoint bleeding is often used as an indicator of reaching the appropriate depth for collagen induction, it’s not always necessary or desirable, especially for superficial treatments or sensitive skin.
- Treat Each Area: Treat one section at a time (e.g., forehead, peri-orbital, nose, peri-oral, chin, and cheeks). Follow these treatment directions: 4 stripes – vertical, horizontal, diagonal right, and diagonal left. Adjust the needle depth according to the treatment area and desired endpoint.
- Maintain Skin Hydration:
- Reapply serum as needed during the procedure to maintain moisture and prevent dragging and tearing of the skin.
- End of Treatment:
- Switch off the pen and retract the needle cartridge. Immediately dispose of the cartridge in a sharps container.
- Clean the pen following the manufacturer’s instructions and unplug the power cord.
Post-Treatment Care
- Immediate Care:
- Wipe off any traces of blood with sterile gauze.
- Apply a calming mask for 15-20 minutes or use a damp, cold gauze to soothe the skin.
- Photographic Documentation:
- Take post-treatment photographs of the treated area for comparison.
- Post-Treatment Application:
- Apply a repair cream and a broad-spectrum sunblock with SPF 30 or higher.
- Patient Instructions:
- Provide detailed post-treatment care instructions, including avoidance of sun exposure, makeup, strenuous exercise, and certain skincare products (e.g., retinoids, AHAs, BHAs) for the specified duration.
- Inform the patient about the stages of healing and what to expect.
- Advise the patient on what to do if anticipated side effects worsen or unexpected issues arise.
Specific Techniques for Various Areas
- Facial Areas:
- Divide the face into quadrants for more precise and uniform microneedling coverage (e.g., left upper, left lower, right upper, right lower).
- While dividing the face into quadrants can be helpful for organizing the treatment, it’s not the only approach. Some practitioners may prefer to treat the entire face as a whole or focus on specific areas of concern. The choice of technique often depends on the individual’s needs and the practitioner’s experience.
- Use gentle traction of the skin to facilitate smooth delivery of microneedles.
- Deep Rhytides or Scars:
- Utilize a “rocking” or “stamping” technique to increase the density of microneedling channels.
- Aim for uniform pinpoint bleeding as the clinical endpoint for these areas.
- Sterilization and Infection Control:
- Use ice water-soaked sterile gauze to remove excess blood and hyaluronic gel.
- Avoid using tap water due to potential contamination risks.
- Apply gentle pressure with dry sterile gauze if bleeding persists.
- Hyaluronic Acid Gel Application:
- Apply a thin layer of hyaluronic acid gel post-treatment and allow it to dry.
Final Steps
- Disposal and Cleaning:
- Dispose of all used materials appropriately.
- Clean and sterilize reusable equipment according to standard procedures.
- Patient Follow-Up:
- Schedule follow-up appointments to monitor healing and results.
- Ensure the patient knows how to contact the clinic for any concerns or complications.
Pain Management Strategies
Pain perception varies among patients. Applying a topical anesthetic cream 30 to 60 minutes before the procedure can significantly reduce discomfort. The selection of anesthetic should be based on the patient’s allergy, the treatment area’s size and the patient’s pain threshold. While topical anesthetic creams are commonly used and effective for pain management during microneedling, other options are available, such as nerve blocks or cooling devices. The choice of pain management strategy should be individualized based on the patient’s preferences, medical history, and the specific treatment plan.
Handling Sensitive Skin Areas
Sensitive areas, such as the forehead, near the eyes, and the upper lip, require special attention due to thinner skin and higher nerve density. In these regions, a shorter needle length and extra care are essential to minimize discomfort and prevent damage. Adjusting the pressure and speed of the microneedling device can also help in managing sensitivity in these areas.
Chapter 6: Post-procedure Care and Patient Instructions
Immediate Post-procedure Care
After a microneedling session, the skin typically appears red and may feel warm and tight, like a sunburn. Immediate post-procedure care focuses on soothing these symptoms and supporting the skin’s healing process:
- Hydration and Calming Agents: Apply a serum or cream rich in hyaluronic acid or other calming agents immediately after the procedure to hydrate and soothe the skin.(NOTE: While hyaluronic acid is commonly used and beneficial for post-microneedling hydration, applying it immediately after the procedure might not be ideal. Some studies suggest that it’s best to wait a few hours or even a day before applying hyaluronic acid or other potentially occlusive products, as this allows the microchannels created by microneedling to close and reduces the risk of irritation or infection.)
- Cooling: Applying a cool compress (not ice) can help reduce redness and swelling.
- Protection: Advise patients to avoid direct sun exposure and to use a broad-spectrum sunscreen with an SPF of 30 or higher. Sun protection is crucial to prevent hyperpigmentation, especially in the first few weeks post-treatment.
Homecare Instructions for Patients
Proper homecare is vital for the healing process and to maximize the benefits of microneedling:
- Gentle Skincare: Patients should use a gentle cleanser and moisturizer to avoid irritating the treated area. Harsh products, including those containing retinoids or acids, should be avoided for at least a week after the procedure.
- Avoid Excessive Heat: Hot showers, saunas, and strenuous exercise that may increase skin temperature and induce sweating should be avoided for the first 24-48 hours post-treatment.
- Sun Protection: Emphasize the importance of applying sunscreen daily to protect the skin from UV damage.
- No Makeup: Advise patients to avoid applying makeup for at least 24 hours after the procedure to prevent clogging the microchannels created by microneedling.
Managing Side Effects and Complications
While microneedling is considered safe, some patients may experience side effects such as bruising, peeling, infection, or post-inflammatory hyperpigmentation. A review by Alster and Graham (2018) provides guidance on managing these potential side effects:
- Bruising and Swelling: These are usually mild and resolve within a few days. Arnica gel can be applied to reduce bruising.
- Peeling: A mild moisturizer can help manage skin flaking without causing further irritation.
- Infection: Though rare, if signs of infection (increased redness, swelling, or pus) occur, patients should be instructed to contact the clinic immediately.
- Hyperpigmentation: Patients with darker skin tones are at higher risk. Using a melanin-inhibiting product pre- and post-treatment can help reduce this risk.
Follow-up Schedule
Scheduling follow-up visits is crucial to monitor the healing process and assess the treatment’s effectiveness. A typical follow-up schedule may include:
- Initial Check-up: 1 week post-procedure to evaluate the skin’s initial healing.
- Subsequent Visits: 4-6 weeks post-treatment to determine the need for additional sessions.
Multiple sessions, usually 3-6, spaced 4-6 weeks apart, may be necessary to achieve the desired results, depending on the skin condition being treated and the individual’s response to the treatment.
Chapter 7: Combination Therapies and Advanced Techniques
Combining Microneedling with Topical Treatments
Microneedling’s ability to enhance the transdermal delivery of topical agents has been a significant focus of research, offering synergistic benefits for various skin conditions:
- Growth Factors and Peptides: Applying growth factors or peptides immediately after microneedling can accelerate healing and boost collagen production.
- Vitamin C and Antioxidants: Vitamin C, known for its antioxidant properties and role in collagen synthesis, is another popular adjunct to microneedling, improving skin brightness and reducing pigmentation when applied topically post-procedure. (NOTE: The micro-channels created by microneedling can increase skin permeability, potentially leading to irritation or adverse reactions when certain topical agents, including Vitamin C, are applied immediately after the procedure. Some studies suggest waiting a few hours or even a day before applying Vitamin C to allow the skin to heal and reduce the risk of irritation.)
- Hyaluronic Acid: Due to its hydrating properties, hyaluronic acid is frequently used post-microneedling to soothe and moisturize the skin, enhancing the procedure’s rejuvenating effects.
Integration with Other Aesthetic Procedures
Microneedling can be combined with other aesthetic treatments for enhanced results:
- Platelet-Rich Plasma (PRP): PRP involves using the patient’s own platelets to promote healing and tissue regeneration. When used in conjunction with microneedling, PRP has been shown to significantly improve outcomes in acne scar treatment and skin rejuvenation.
- Lasers and Light Therapy: Combining microneedling with laser treatments or LED light therapy can address a broader range of skin concerns, from pigmentation disorders to skin laxity. Sequential treatments may be planned, with microneedling enhancing the effects of laser therapy by facilitating deeper penetration and more effective targeting of skin issues. Performing microneedling immediately before or after laser therapy can increase the risk of complications, such as prolonged erythema, hyperpigmentation, or scarring. It’s generally recommended to wait at least a few weeks between these procedures.
Recent Advances and Research Insights
The field of microneedling continues to evolve, with ongoing research into new applications and technology:
- Radiofrequency Microneedling: This advanced technique combines microneedling with radiofrequency energy to tighten skin and improve texture. The radiofrequency energy is delivered through the microneedles, enhancing collagen and elastin production at deeper skin layers.
- Nanotechnology: Recent innovations include the development of nanoneedles, which can deliver active ingredients to precise depths in the skin, offering targeted treatment for various dermatological conditions with minimal discomfort and downtime. However, their use in microneedling for cosmetic purposes is still in the early stages of research and development. Further studies are needed to establish their safety, efficacy, and optimal use in dermatological treatments.
Chapter 8: Practice Management and Ethical Considerations
Incorporating Microneedling Services into Practice
As microneedling becomes an increasingly sought-after treatment in cosmetic dermatology, practices must consider several factors to successfully incorporate this service:
- Training and Certification: Ensure practitioners are properly trained and certified in microneedling techniques. Training programs should cover the science behind the procedure, hands-on techniques, and patient safety protocols.
- Quality Equipment: Invest in high-quality, FDA-approved microneedling devices to ensure patient safety and treatment efficacy. The selection of equipment can impact the results and patient satisfaction.
- Regulatory Compliance: Stay informed about state and federal regulations governing the use of microneedling devices in practice. Compliance with these regulations is essential to operate legally and ethically.
Expert Commentary and Best Practices
Experts in dermatology and aesthetic medicine have contributed insights into optimizing microneedling treatments:
- Patient Selection: Choosing the right candidates based on skin type, condition severity, and medical history is crucial for achieving optimal outcomes.
- Customization of Treatment: Adjusting needle depth, the number of passes, and combining therapies based on individual patient needs can enhance results.
- Post-Treatment Care: Emphasizing the importance of sunscreen, gentle skincare, and avoidance of irritants post-procedure to support healing and maximize benefits.
- Safety Protocols: Maintaining strict hygiene and sterilization standards to prevent infections and complications.
Setting Patient Expectations
Effective communication is crucial in setting realistic expectations for microneedling outcomes:
- Consultation Process: Use the initial consultation to educate patients about the procedure, expected outcomes, potential side effects, and the number of sessions required.
- Visual Aids: Before-and-after photos of previous patients (with their consent) can be helpful in illustrating potential outcomes.
- Written Materials: Provide patients with brochures or links to reputable websites for additional information on microneedling.
Legal and Ethical Issues in Cosmetic Dermatology
Microneedling practitioners must navigate a range of legal and ethical considerations:
- Informed Consent: Obtain written informed consent from patients after fully explaining the procedure’s risks, benefits, and alternatives. This process is critical for ethical practice and legal protection.
- Advertising Practices: Ensure marketing materials for microneedling services are truthful, do not make unrealistic promises, and comply with advertising standards set by medical boards and associations.
- Privacy and Confidentiality: Protect patient privacy and confidentiality in accordance with HIPAA and other relevant laws. This includes secure storage of patient photos and records.
Scientific References Summary
- Alster, T.S., & Graham, P.M. (2018). “Microneedling: A Review and Practical Guide.” Dermatologic Surgery. This review provides a comprehensive guide on microneedling procedures, highlighting practical approaches and summarizing the technique’s efficacy and safety.
- Alster, T.S., & West, T.B. (1998). “Effect of Topical Vitamin C on Postoperative CO2 Laser Resurfacing Erythema.” Dermatologic Surgery. This study investigates the impact of topical Vitamin C on reducing erythema after laser resurfacing, underscoring the antioxidant’s beneficial effects in post-procedure healing.
- Asgari, M., et al. (2016). “A Comparative Study of Microneedling with Platelet-Rich Plasma Plus Tranexamic Acid Versus Microneedling with Platelet-Rich Plasma Only in Treating Atrophic Post Acne Scars: A Split Face Study.” Journal of Cosmetic Dermatology. This study examines the efficacy of combining microneedling with PRP and tranexamic acid for treating atrophic acne scars, showing improved outcomes with the combination therapy.
- Aust, M.C., et al. (2008). “Percutaneous Collagen Induction: Minimally Invasive Skin Rejuvenation without Risk of Hyperpigmentation—Fact or Fiction?” Plastic and Reconstructive Surgery. The article discusses the benefits of microneedling for skin rejuvenation, particularly highlighting its low risk of causing hyperpigmentation compared to other invasive procedures.
- Camirand, A., & Doucet, J. (1997). “Needle Dermabrasion.” Aesthetic Plastic Surgery. One of the early studies discussing the concept of using needles for skin rejuvenation, setting the stage for modern microneedling techniques.
- Dayan, S.H., et al. (2019). “Ethics in Aesthetic Medicine and Plastic Surgery: A Review and Proposed Practical Approach.” Aesthetic Surgery Journal. This review addresses the ethical considerations in aesthetic medicine, including the need for honest advertising and patient consent.
- Dhurat, R., et al. (2013). “A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study.” International Journal of Trichology. This pivotal study demonstrates the effectiveness of microneedling in enhancing hair regrowth in patients with androgenetic alopecia, especially when combined with topical treatments.
- El-Domyati, M., et al. (2015). “Microneedling Therapy for Atrophic Acne Scars: An Objective Evaluation.” Journal of Clinical and Aesthetic Dermatology. This research provides objective evidence on the efficacy of microneedling in improving the appearance of atrophic acne scars.
- Fabbrocini, G., et al. (2016). “Collagen Induction Therapy for the Treatment of Acne Scars.” Dermatologic Surgery. This study explores the effectiveness of microneedling, specifically collagen induction therapy, in treating acne scars, showing significant improvements in skin texture and scar appearance.
- Hantash, B.M., & Renton, B. (2009). “Pilot Clinical Study of a Novel Minimally Invasive Bipolar Microneedle Radiofrequency Device.” Lasers in Surgery and Medicine. This clinical study introduces a novel approach combining microneedling with radiofrequency energy, indicating its potential for skin tightening and rejuvenation.
- Kluger, N., Koljonen, V. (2017). “Consent and Ethical Considerations for Dermatologic Surgery.” Journal of the American Academy of Dermatology. The article emphasizes the importance of informed consent in dermatological procedures, including cosmetic interventions like microneedling.
- Lee, W.R., et al. (2011). “The Skin Penetration of Quantum Dots Delivered by Microneedle Arrays and Its Implication for Transdermal Delivery.” Journal of Controlled Release. This study explores the use of microneedle arrays for delivering quantum dots into the skin, highlighting the potential for targeted drug delivery.
- Majid, I. (2010). “Microneedling Therapy in Atrophic Facial Scars: An Objective Assessment.” Journal of Cutaneous and Aesthetic Surgery. Majid’s work provides objective data on the benefits of microneedling for atrophic facial scars, showing significant improvements in skin texture and scar depth.
- Morton, L.M., Phillips, T.J. (2016). “HIPAA Compliance and Dermatology: An Overview of the Health Insurance Portability and Accountability Act.” Journal of the American Academy of Dermatology. This article provides an overview of HIPAA regulations relevant to dermatological practice.
- Na, J.I., et al. (2012). “Combination of Microneedling and Fractional Laser Therapy for the Treatment of Acne Scars: A Pilot Study.” Journal of Dermatological Treatment. This study evaluates the combined effects of microneedling and fractional laser therapy on acne scars, demonstrating enhanced treatment outcomes.
- Singh, A., & Yadav, S. (2016). “Microneedling: Advances and Widening Horizons.” Indian Dermatology Online Journal. This article reviews the advances in microneedling technology and its expanding applications in dermatology.
- Sharad, J. (2013). “Microneedling with Dermaroller.” Journal of Cutaneous and Aesthetic Surgery. This paper provides insights into the techniques and outcomes of microneedling using a dermaroller, highlighting its effectiveness for various skin conditions.
